Post Procedure Care
The first hour after the procedure is critical to observe the patient for any complications after their cardiac catheterization.
- Identify whether the patient had a diagnostic or interventional cardiac catheterization. Interventional procedures have a significantly higher rate of complications compared to diagnostic procedures.
- Identify the access site. Radial or Femoral. Arterial or venous.
- Did the patient receive any anticoagulation during the procedure? If anticoagulation was given, the patient is at a higher risk of bleeding.
- Identify how access hemostasis was obtained. Manual compression or closure device.
- Be aware of the results of the procedure - presence of coronary heart disease - presence of left ventricular dysfunction.
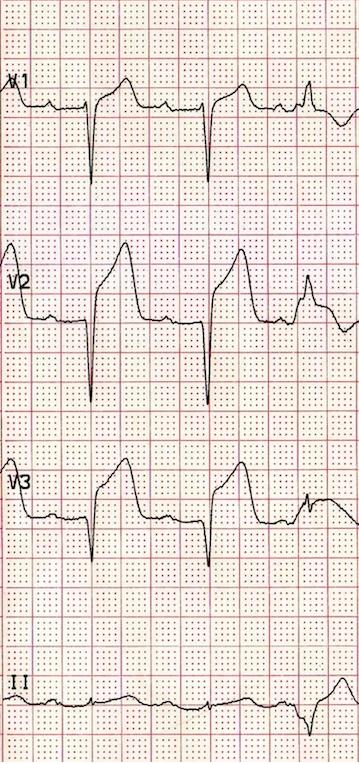
- Review ECG and compare with baseline rhythm.
- Review what medications were given during the catheterization.
- Perform Vital Sign Assessment and Access Site Assessment every 15 minutes for the first hour, then every 30 minutes for the 2nd hour, then every hour for the remainder of their recovery. Be sure to follow your institutional guidelines for frequency of vital sign assessment.
- For femoral access: keep patient bedrest for recommended number of hours with head and legs flat in bed. Patient can be reposition side to side to provide comfort, as long as the affected extremity is maintained in a straight alignment with the torso. After the 1st hour, it may be safe to raise the HOB up to 30 degrees
- For radial access: keep wrist imobilized for recommended numbef of hours with an armboard. Minimize activity the requires use of affected extremkty. The HOB can be raised to patients desired level.
Puncture Site Assessment
Bleeding - check access dressing for oozing or bleeding (especially after vomiting or coughing).
Hematoma - check access site for swelling, redness and tenderness.
Assessment of Potential Complications
Retroperitoneal Bleeding - this is one of the most critical complications that can occur post cardiac catheterization. Assess vital signs for tachycardia and hypotension. Retroperitoneal bleeding will lead to vascular volume depletion. Assess for abdominal pain, groin pain, and lower back pain. Observe for diaphoresis. Monitor blood results for decreasing hematocrit level. Be prepared for emergent critical care!
Arrhythmias - review patients baseline rhythm and ensure that it is in sinus rhythm or what is normal for the patient.
Vascular thrombus - observe the affected extremity for color, temperature, sensation and distal pulses. Thrombus can result in a pale, cool, tingling extremity with diminished or absent pulses.
Contrast Induced Nephropathy (CIN) - impaired renal function with a 25% increase in serum creatinine levels. Pre-existing renal impairment is at a greater risk for CIN. PO and IV hydration should be administered: Encourage the patient to drink 2,500 mL of water over the next 24 hours. The patient should be given IV hydration of 250 mL/hour x 4 hours. Be careful with hydrating the patient with a history of congestive heart failure
Patient Education
- Patient will need to rest for the next 3 days and avoid heavy lifting and strenuous activity during this time.
- For the next 24 hours: do not drive, avoid signing legal documents, and avoid stairs.
- Patients should avoid tub bathing or swimming until the puncture site is healed.
- The puncture site dressing should be changed every 24 hours until a scab has formed.
- The patient may experience soreness at the puncture site, but if it gets worse, they should notify their physician.
- If the puncture site begins to bleed, hold pressure over the site and call 911 or available emergency number.
References
- Timbly, B., & Smith, N. (2004)
Essentials of Nursing: Care of Adults and Children . London, Lippincott Williams & Wilkins.